|
Case Report
Clinical investigation of Ramsay–Hunt syndrome with glossopharyngeal and vagal nerve involvement
1 Professor, Department of Health, Faculty of Health Sciences, Tsukuba University of Technology, Tsukuba, Ibaraki, Japan
2 Professor, Department of Neurology, Faculty of Medicine, University of Tsukuba, Tsukuba, Japan
3 Professor, Department of Radiological Technology, Tsukuba International University, Ibaraki, Japan
Address correspondence to:
Nobuko Shiraiwa
4-12-7 Kasuga, Tsukuba, Ibaraki 305-8521,
Japan
Message to Corresponding Author
Article ID: 100019N06NS2024
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Shiraiwa N, Tamaoka A, Ohkoshi N. Clinical investigation of Ramsay–Hunt syndrome with glossopharyngeal and vagal nerve involvement. Edorium J Neurol 2024;9(1):5–8.ABSTRACT
Introduction: Ramsay–Hunt syndrome is a peripheral facial nerve palsy accompanied by an erythematous vesicular rash in the ear (zoster oticus). Although involvement of the facial and vestibulocochlear nerves is typical in Ramsay–Hunt syndrome, multiple cranial neuropathies are rare, and are often associated with poorer prognosis and systemic complications. Here, we evaluated the clinical course of a rare case of Ramsay–Hunt syndrome associated with glossopharyngeal and vagal nerve disorders.
Case Report: A 75-year-old man presented with right facial paralysis, hoarseness, and dysphagia, leading to the diagnosis of Ramsay–Hunt syndrome with glossopharyngeal and vagal nerve disorders. The time between onset and initiation of antiviral drug administration was six days. Five years earlier, the patient had developed deafness on the same side along with dizziness. Facial paralysis and dysphagia improved nine months after onset; however, deafness, dizziness, and hoarseness persisted. The possibility of vestibulocochlear nerve palsy due to Zoster sine herpete was therefore considered.
Conclusion: Ramsay–Hunt syndrome with multiple cranial neuropathies is rare and is usually associated with a poorer prognosis. In this case, facial paralysis and dysphagia improved nine months after onset;however, deafness, dizziness, and hoarseness persisted. Therefore, attention must be paid to unilateral cranial nerve disorders, including Zoster sine herpete, during the assessment process.
Keywords: Glossopharyngeal nerve, Herpes zoster, Ramsay–Hunt syndrome, Vagus nerve, Zoster sine herpete
INTRODUCTION
Ramsay–Hunt syndrome (RHS) is a peripheral facial nerve palsy accompanied by an erythematous vesicular rash in the ear (zoster oticus). This condition is caused by reactivation of the varicella-zoster virus (VZV) in the geniculate ganglion of the facial nerve [1]. Although involvement of the facial and vestibulocochlear nerves is typical in RHS, multiple cranial neuropathies are rare, and are often associated with a poorer prognosis and systemic complications [2],[3],[4],[5],[6],[7]. We evaluated the clinical course of a rare case of RHS associated with glossopharyngeal and vagal nerve disorders.
CASE REPORT
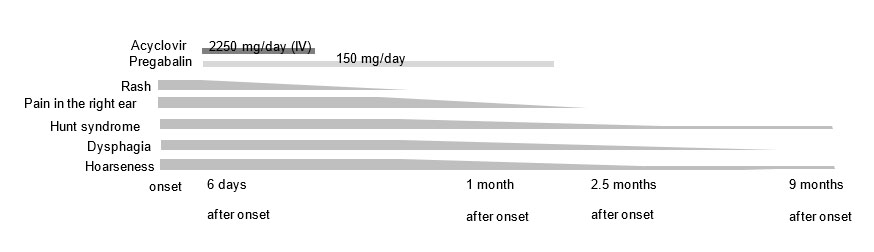
A 75-year-old man with treated hypertension presented with a sore throat and pain in the right ear. When he consulted a doctor the next day, where a cold was suggested (Figure 1). Three days later, the patient visited the hospital again and blisters were detected on the right pinna; he was diagnosed with otitis externa. He visited another hospital the next day owing to the spread of the rash to the right side of his face and swelling of the right auricle and was diagnosed with herpes zoster (HZ) six days after symptom onset. Alongside a rash featuring blisters that extended from the second branch of the right trigeminal nerve to the C2 region and ear canal, there were paralysis of the right peripheral facial nerve, hoarseness, and dysphagia. Pustules in the right ear tested positive for the VZV antigen. Serum analysis by complement fixation test for VZV antibody was positive (<x4 [–]). Therefore, anti-viral treatment with valaciclovir 3000 mg/day was initiated. The next day, the patient was admitted to the hospital and administered 750 mg of intravenous acyclovir every 8 h for 10 days.
Subsequently, one month later, the patient visited the Neurology Department of our clinic. Physical examination revealed crusting of the subcutaneous rash on the right pinna and back of the head, pain in the pinna, and paralysis of the right peripheral facial nerve (Yanagihara method paralysis score, 12 points). In addition, deafness on the same side, dizziness, hoarseness, and dysphagia (swallowing solid food was difficult) were observed. Furthermore, the patient had experienced deafness of the right side and dizziness for five years and had been diagnosed with sudden right sensorineural hearing loss at 70 years of age. At that time, he showed no rash on his ear or mouth, and was prescribed steroids; however, his hearing did not improve.
This was determined to be a relatively rare case of RHS combined with hoarseness and dysphagia due to glossopharyngeal and vagal nerve paresis. Pregabalin treatment was initiated for auricular pain, and rehabilitation was initiated for facial paralysis. Hoarseness and dysphagia were managed by the Department of Otolaryngology.
Auricular pain improved 2.5 months later, and pregabalin treatment was discontinued. Approximately nine months after the onset, the patient recovered from facial paralysis and dysphagia almost completely. No pathological synkinesis, facial convulsions, crocodile tears, or stiffness were observed. The facial paralysis score was 40; nevertheless, deafness, dizziness, and hoarseness persisted.
DISCUSSION
Lower cranial nerve palsies have been found to be less frequent in patients with RHS caused by VZV [8],[9]. Tsau et al. [8] summarized the characteristics of 330 patients with HZ infection and cranial nerve involvement and reported that 0.9% of patients had glossopharyngeal and vagus nerve involvement, in addition to facial palsy and vestibulocochlear nerve disorders. Gunbey et al. [9] described a patient with rare polyneuropathy of VZV infection, confirmed radiologically through magnetic resonance imaging (MRI), which revealed the involvement of cranial nerves VII, IX, and X.
Our patient was identified as having a relatively rare case of RHS combined with hoarseness and dysphagia due to a lower cranial nerve disorder. Varicella-zoster virus infection should be considered, even in patients with unilateral palsy of the lower cranial nerves associated with laryngeal paralysis.
Zoster sine herpete (ZSH) is a term used to describe typical dermatomal pain due to VZV in the absence of a characteristic rash [10],[11]. Our patient experienced deafness on the same side and dizziness for five years and had no ear or mouth rash during that time. Hence, we considered the possibility that our patient had vestibulocochlear nerve palsy due to ZSH.
Mondelli et al. [12] reported that oral treatment with aciclovir reduced peripheral sensory axonopathy due to ganglion damage and the risk of spreading to the anterior roots and spinal motor neurons. Regular antiviral therapy within 72 h of skin rash appearance is believed to be able to substantially reduce pain over time, as well as minimize the risk of other related complications [13],[14]. On this basis, our patient was not administered antiviral drugs within 72 h of onset. In the early stages of RHS, the typical shingles rash often occurs in areas that are difficult to notice, such as the ear canal. This patient could have had the rash in his ear canal on day he presented with pain in the right ear. Therefore, it is important not to overlook the rash to avoid delays in diagnosis of RHS. Approximately nine months after onset, his right facial palsy and dysphagia improved almost completely; however, deafness, dizziness, and hoarseness persisted.
CONCLUSION
Ramsay–Hunt syndrome with multiple cranial neuropathies is rare and is usually associated with a poorer prognosis. In the case reported herein, facial paralysis and dysphagia improved nine months after onset; however, deafness, dizziness, and hoarseness persisted. Our findings emphasize the importance of vigilance for unilateral cranial nerve disorders, including ZSH, during the assessment process.
REFERENCES
1.
Sweeney CJ, Gilden DH. Ramsay Hunt syndrome. J Neurol Neurosurg Psychiatry 2001;71(2):149–54. [CrossRef]
[Pubmed]

2.
Ananthapadmanabhan S, Soodin D, Sritharan N, Sivapathasingam V. Ramsay Hunt syndrome with multiple cranial neuropathy: A literature review. Eur Arch Otorhinolaryngol 2022;279(5):2239–44. [CrossRef]
[Pubmed]

3.
Arya D, Bajaj T, Gonzalez J, Elkin R. Ramsay Hunt syndrome with multiple cranial neuropathy in an human immunodeficiency virus (HIV) patient. Am J Case Rep 2018;19:68–71. [CrossRef]
[Pubmed]

4.
Shinha T, Krishna P. Ramsay Hunt syndrome and zoster laryngitis with multiple cranial nerve involvement. IDCases 2015;2(2):47–8. [CrossRef]
[Pubmed]

5.
Shim HJ, Jung H, Park DC, Lee JH, Yeo SG. Ramsay Hunt syndrome with multicranial nerve involvement. Acta Otolaryngol 2011;131(2):210–5. [CrossRef]
[Pubmed]

6.
Coleman C, Fozo M, Rubin A. Ramsay Hunt syndrome with severe dysphagia. J Voice 2012;26(1):e27–8. [CrossRef]
[Pubmed]

7.
Morelli N, Mancuso M, Cafforio G, et al. Ramsay-Hunt syndrome complicated by unilateral multiple cranial nerve palsies. Neurol Sci 2008;29(6):497–8. [CrossRef]
[Pubmed]

8.
Tsau PW, Liao MF, Hsu JL, et al. Clinical presentations and outcome studies of cranial nerve involvement in herpes zoster infection: A retrospective single-center analysis. J Clin Med 2020;9(4):946. [CrossRef]
[Pubmed]

9.
Gunbey HP, Kutlar G, Aslan K, Sayit AT, Incesu L. Magnetic resonance imaging evidence of varicella zoster virus polyneuropathy: Involvement of the glossopharyngeal and vagus nerves associated with Ramsay Hunt syndrome. J Craniofac Surg 2016;27(3):721–3. [CrossRef]
[Pubmed]

10.
Kennedy PGE. Zoster sine herpete: It would be rash to ignore it. Neurology 2011;76(5):416–7. [CrossRef]
[Pubmed]

11.
Kennedy PGE, Gershon AA. Clinical features of varicella-zoster virus infection. Viruses 2018;10(11):609. [CrossRef]
[Pubmed]

12.
Mondelli M, Romano C, Passero S, Porta PD, Rossi A. Effects of acyclovir on sensory axonal neuropathy, segmental motor paresis and postherpetic neuralgia in herpes zoster patients. Eur Neurol 1996;36(5):288–92. [CrossRef]
[Pubmed]

13.
Meng Y, Zhuang L, Jiang W, Zheng B, Yu B. Segmental zoster paresis: A literature review. Pain Physician 2021;24(3):253–61.
[Pubmed]

14.
O’Connor KM, Paauw DS. Herpes zoster. Med Clin North Am 2013;97(4):503–22, ix. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
We would like to thank Editage (www.editage.jp) for English language editing.
Author ContributionsNobuko Shiraiwa - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Akira Tamaoka - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Norio Ohkoshi - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2024 Nobuko Shiraiwa et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.