|
Case Report
Extensive dural calcification in a young female patient: A case report
1 Neurology Department, King Abdulaziz bin Saud University for Health Sciences (KSAU-HS), King Abdulaziz Medical City (KAMC), Riyadh, Kingdom of Saudi Arabia
Address correspondence to:
Naser Alotaibi
Neurology Department, King Abdulaziz bin Saud University for Health Sciences (KSAU-HS), King Abdulaziz Medical City (KAMC), Riyadh,
Kingdom of Saudi Arabia
Message to Corresponding Author
Article ID: 100020N06NA2024
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Alotaibi N. Extensive dural calcification in a young female patient: A case report. Edorium J Neurol 2024;9(2):1–4.ABSTRACT
Introduction: Dural calcification is most observed in older adults. However, idiopathic extensive dural calcification is rare in young individuals, often raising concerns for potential underlying secondary diseases or disorders. Dural calcification is typically categorized into physiological (age-related and idiopathic) and pathological types (associated with underlying conditions) linked to metabolic and genetic factors.
Case Report: We report distinctive idiopathic extensive dural calcification in an asymptomatic young adult female with no known pathological or metabolic predispositions.
Conclusion: The presence of this condition in young, healthy adults without any identifiable etiologies is exceptionally uncommon. This case represents a rare instance of such extensive dural calcification in a healthy young adult, contributing a unique addition to the medical literature on this rare entity.
Keywords: Calcification, Dural, Extensive, Idiopathic
INTRODUCTION
Extensive dural calcification occurs when calcium minerals are deposited in the dura matter. More common is intracranial calcification, defined by Dhamodaran et al. as a deposition of either calcium or iron in the blood vessels of the brain structures [1]. The incidence of dural calcification increases with aging and degenerative changes [2].
Brain computed tomography (CT) scan is the most accurate method for detecting intracranial calcifications. Computed tomography scan findings can be categorized as either pathologic or physiologic/age-related.
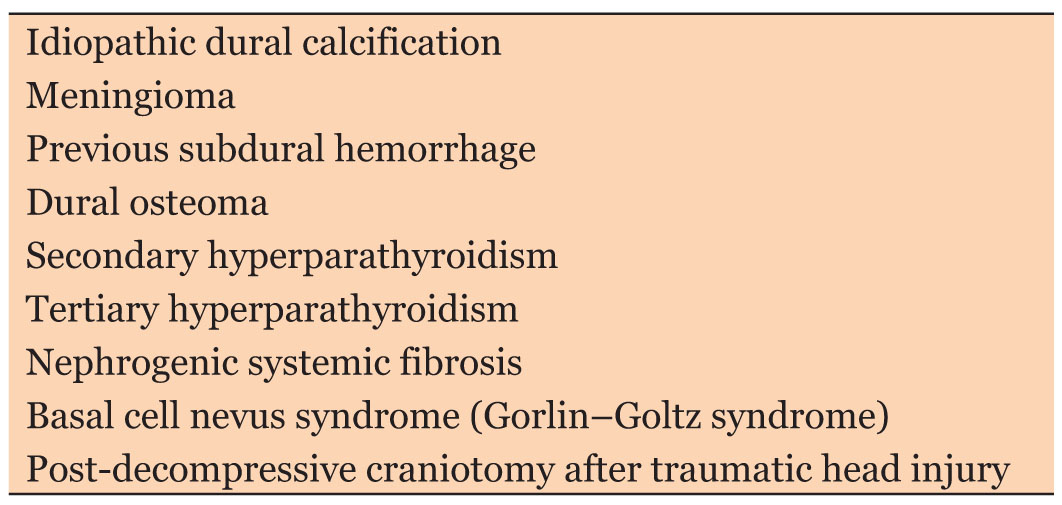
Determining the cause of intracranial calcifications can be challenging. Depending on the patient’s age, these calcifications might be categorized as physiological, but other factors can sometimes cause them. To facilitate the differential diagnosis as shown in Table 1, it is important to consider the anatomical location, distribution, calcification dimensions, and morphology of these calcifications, along with the patient’s age group and clinical history.
In this report, we discuss one of the rare cases of extensive dural calcification in a young female patient and highlight the clinical history, clinical findings, and differential diagnosis, for this pathology.
CASE REPORT
A 35-year-old woman with an unremarkable past medical history had been evaluated in the neurology outpatient clinic for persistent daily headache attacks over the last four months. The headache attacks were typical migraines in nature. It was frequent, mild to moderate, throbbing, and persisted most of the day. The patient described it as a unilateral right-sided headache. She also reported eye pain, nausea, phonophobia, and photophobia. She denied any history of seizure, motor, or sensory symptoms. Family history revealed no neurological, metabolic, or genetic disorders. She tried different pain-controlling medications, including acetaminophen and non-steroidal anti-inflammatory drugs, with minimum response. Clinical examination revealed normal physical and neurological evaluation.
Investigations
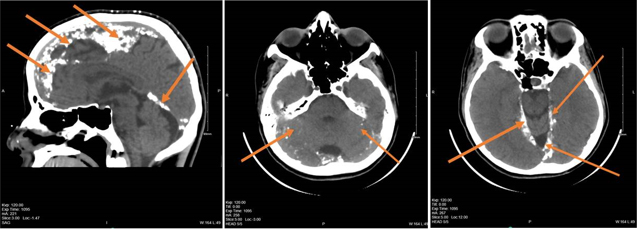
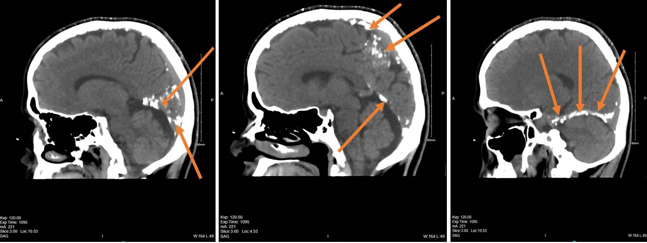
Several basic investigations and blood tests were performed, including a complete blood count and a brain CT scan, which showed extensive calcification along the falx cerebri and tentorium cerebelli (Figure 1 and Figure 2). This required further blood tests, including all metabolic workups, calcium, phosphorous, magnesium, renal and liver functions, and levels of thyroid-stimulating hormone and parathyroid hormone. All results were within the normal range, and nothing abnormal was detected.
Further, the image of the brain with brain magnetic resonance imaging (MRI) was conducted and confirmed extra-axial calcification but with no parenchymal calcification and no gross parenchymal abnormality.
Differential Diagnosis
Treatment, Outcome, and Follow-Up
The patient was reassured that the CT scan abnormality is related to benign idiopathic incidental dural calcification and that her headache is likely the primary type, classified as moderate chronic migraine. She was treated with a daily prophylactic dose of tricyclic antidepressant medication, amitriptyline 25 mg, for three months, combined with abortive triptan medication for severe attacks. A follow-up visit revealed a significant reduction in her headache frequency and severity of more than 50% as measured by Migraine Disability Assessment Questionnaire (MIDAS).
DISCUSSION
We report this rare case using data from our neurology clinic through direct patient interaction, follow-up visits, and electronic medical records.
A thorough literature review was conducted using PubMed, Medline, and other medical databases to find similar reported cases and related pathology publications.
Dural calcifications occur in only 1% of the population aged between 29 and 87 [1]. Furthermore, extensive dural calcification is a rare phenomenon often related to secondary metabolic disorders, genetics, or age-related factors. However, the idiopathic condition in young patients without an obvious cause is considered a rare clinical presentation.
According to Saade et al., age-related intracranial calcifications, which are likely physiologic, have no known causes. They are usually found in the pineal gland, choroid plexus, habenula, falx cerebri, tentorium cerebelli, and basal ganglia. The pattern of these calcifications can be coarse and compact, punctate, or curvilinear
In addition, physiologic/age-related calcifications are generally discovered incidentally during a brain CT scan, as found with our patient. According to Saade et al., dural calcification cases are more common in male patients in their 50s [4]. However, our patient is a female in her 30s, which is younger than the typical age of onset. Furthermore, Guedes et al. reported that this type of calcification is a typical finding in adult and elderly patients, especially those older than 40. They also reported that the radiological aspects usually appear as an extensive image [5].
Our patient presented with primary headache, likely to be migraine, and thorough laboratory investigations, including calcium and parathyroid hormone, were normal. Further investigation of the brain CT scan revealed extensive calcification along the falx cerebri and tentorium cerebelli, with no brain parenchymal calcification.
In a case reported by Daoud et al., the patient had a medical history of seizures, hydrocephalus, and extensive meningeal calcification located in the falx cerebri. However, despite having normal renal functional test (RFT) and vitamin D levels, the patient experienced seizures and had low serum calcium, high phosphate, and high parathyroid hormone levels. These readings led the medical team to consider the patient who was diagnosed with pseudohypoparathyroidism [6].
Brain tumors and inflammation (meningitis, osteomyelitis following head injury, etc.) have been listed as causes of calcification of the dura mater in previous reports.
Yasuakira Tanaka and Kazuo Takeuchi examine dural calcification, reporting a 14% incidence among 1162 neurological and neurosurgical patients. The study found that calcification primarily occurred in the falx cerebri, tentorium cerebelli, and petro-clinoid ligament. They found the clinical significance, noting that calcification often results from aging, long-term lesion irritation, head injuries, and endocrine disorders. They concluded that dural calcification is less significant than pineal calcification [7].
According to Serindere and Polat, 1000 patients were retrospectively evaluated intracranially for the region of calcifications when they were studied. Those patients were referred to the radiology department for various reasons. They were 431 females and 569 males; they found falx cerebri calcification in (6.2%) and tentorium cerebelli calcification in (0.2%). It is rare to have calcification in these two regions [8]. Serindere and Polat also mentioned that the incidence and co-existence of calcifications increased with age. Tentorium cerebelli calcification did not differ significantly between age groups (p > 0.05) [7]. Khurram et al. further explained that the density of intracranial calcification is not directly related to the patient’s clinical consequences. Instead, the clinical sequelae are more related to the biochemical hypo-calcemia [9].
The common distribution of intracranial calcification was studied in various ways and tried to relate it with age and gender. Kiraz examined retrospectively 1011 (460 females and 551 males) with mean age (39.5 years females and 38.3 years males) patients who were presented at the Emergency Department because of head trauma. He studied the relationship between the age and gender of the patient and the physiological intracranial calcifications. He found that increasing age increases the incidence of calcification intracranial distribution, and dural calcification is (p < 0.001) statistically significant [10].
Dhamodaran found that only 8% of intracranial calcifications are associated with dural calcifications, and the majority are male. The density of calcification was also higher in males than in females [1],[11]. However, Choroid plexus calcifications were concomitantly seen in up to 78.4% of patients with dural calcifications [12].
Extensive dural calcification is a rare condition that usually affects older adults and older people. It is more associated with metabolic and genetic causes, and many patients present with seizures. Detecting extensive dural calcification in young, healthy adults without any metabolic or genetic disorders is unusual.
CONCLUSION
- This case highlights the exceptionally uncommon occurrence of extensive dural calcification in a young, healthy adult without any identifiable etiologies or underlying metabolic or genetic disorders.
- Idiopathic extensive dural calcification is extremely rare among young individuals, and when detected, a thorough chemistry, metabolic, and genetic workup is indicated to rule out secondary causes.
- The presence of idiopathic extensive dural calcification in an asymptomatic young adult underscores the need for awareness and recognition of this rare clinical entity, contributing a unique case to the medical literature.
REFERENCES
1.
2.
Tepe RD, Cakir Karabas H, Erturk AF, Ozcan I. Physiologic intracranial calcifications incidentally detected on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol 2022;134(5):e281–6. [CrossRef]
[Pubmed]

3.
Dorenbeck U, Leingärtner T, Bretschneider T, Krämer BK, Feuerbach S. Tentorial and dural calcification with tertiary hyperparathyroidism: A rare entity in chronic renal failure. Eur Radiol 2002;12 Suppl 3:S11–3. [CrossRef]
[Pubmed]

4.
Saade C, Najem E, Asmar K, Salman R, El Achkar B, Naffaa L. Intracranial calcifications on CT: An updated review. J Radiol Case Rep 2019;13(8):1–18. [CrossRef]
[Pubmed]

5.
Guedes MDS, Queiroz IC, de Castro CC. Classification and clinical significance of intracranial calcifications: A pictorial essay. Radiol Bras. 2020;53(4):273–8. [CrossRef]
[Pubmed]

6.
Daoud MS, Elamin AA, Mohammed AR, Khalid A, Hassan A, Taha A. A patient with extensive meningeal calcification due to pseudohypoparathyroidism: A case report. Authorea 2022. [CrossRef]

7.
Tanaka Y, Takeuchi K. Dural calcification from the neurosurgical point of view. Neurol Med Chir (Tokyo) 1974;14 pt 1:5–10. [CrossRef]
[Pubmed]

8.
Serindere M, Polat G. Intracranial physiological calcifications: A computed tomography study. Imaging 2023;15(1):23–30. [CrossRef]

9.
Khurram R, Khamar R, Mandumula S. Computed tomography findings of diffuse intracranial calcifications in a patient with primary hypoparathyroidism. J Radiol Clin Imaging 2020;3(1):33–7. [CrossRef]

10.
Kiraz M. The relationship with age and gender of intracranial physiological calcifications: A study from Corum, Turkey. Ann Med Res 2021;28(9):1775–80. [CrossRef]

11.
Whitehead MT, Oh C, Raju A, Choudhri AF. Physiologic pineal region, choroid plexus, and dural calcifications in the first decade of life. AJNR Am J Neuroradiol 2015;36(3):575–80. [CrossRef]
[Pubmed]

12.
Yalcin A, Ceylan M, Bayraktutan OF, Sonkaya AR, Yuce I. Age and gender related prevalence of intracranial calcifications in CT imaging; data from 12,000 healthy subjects. J Chem Neuroanat 2016;78:20–4. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Naser Alotaibi - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthor declares no conflict of interest.
Copyright© 2024 Naser Alotaibi. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.